Generalmente los pacientes tienen dudas sobre diversos temas relacionado con el trabajo que realizamos los embriólogos, sobre sus embriones, el desarrollo y la calidad de estos; además de muchos más temas que recogemos a continuación:
¿Qué es el REM? ¿es un factor decisivo para realizar una técnica u otra de Reproducción Asistida?
El REM nos permite conocer el valor de la concentración de espermatozoides y el porcentaje de espermatozoides con movilidad progresiva. No es un factor decisivo en exclusividad, pero en función de esta valiosa información, decidiremos qué técnica de reproducción asistida es la idónea:
- Inseminación artificial (IA): si el REM muestra buenos resultados, es decir, alta concentración y buena movilidad, podremos realizar una IA. Generalmente se recomienda aplicar esta técnica cuando el REM es superior a 3 millones de espermatozoides móviles progresivos.
- Fecundación in vitro (FIV): si la muestra de semen capacitada tiene una concentración de espermatozoides móviles progresivos menor a 3 millones, la inseminación artificial puede no ser efectiva por lo que se recomendará la FIV.
¿Cuántas células tiene que tener un embrión cada día que pasa?
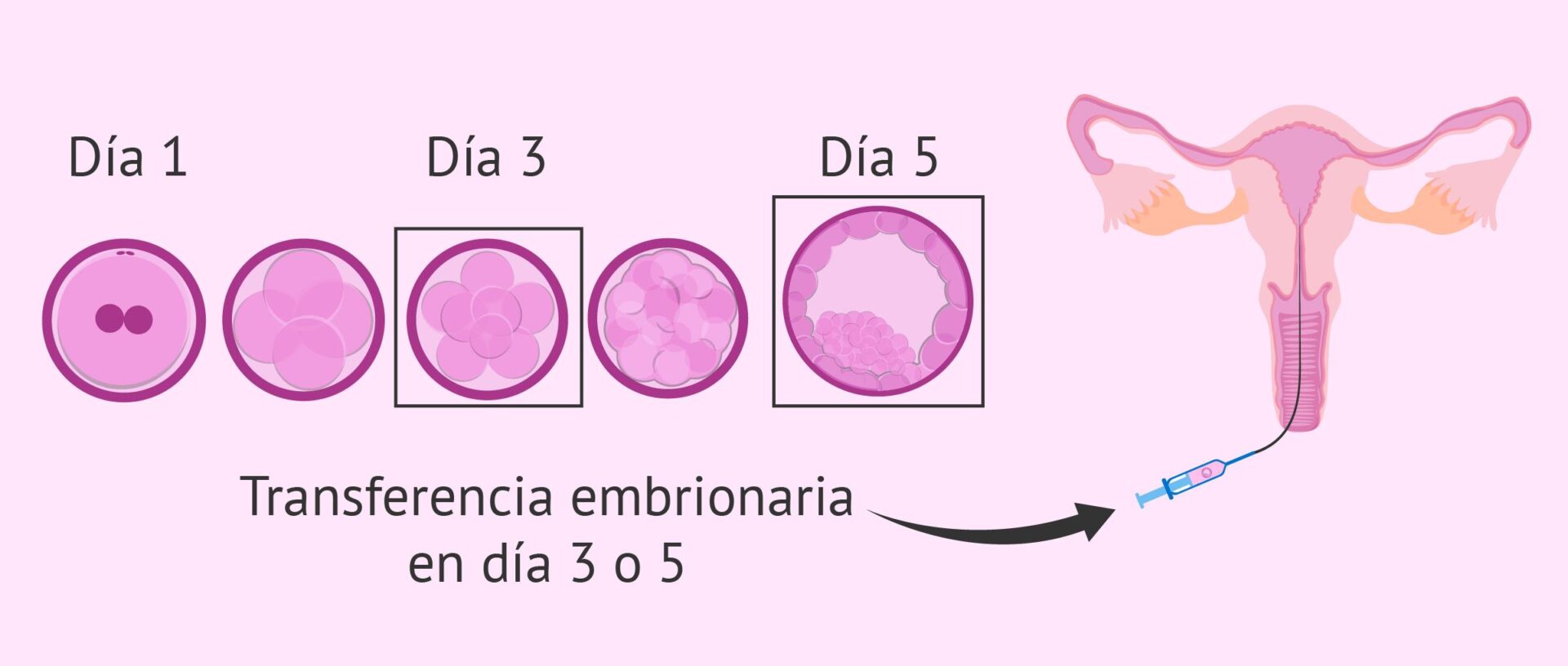
Como hemos dicho anteriormente, contamos como día 0 el mismo día de la punción folicular y por tanto el día que realizamos la FIV/ICSI.
- DÍA 1: visualizaremos la FECUNDACIÓN, es decir, si se ha producido correctamente la unión entre ovulo y espermatozoide. Decimos que un ovulo ha fecundado correctamente cuando vemos dos núcleos (o pronúcleos). Uno de ellos proviene del mismo ovulo y el otro del espermatozoide. Estos pronúcleos contienen en ADN de ambas células. Cuando nos dan la noticia de una “mala fecundación”, es porque algo no ha salido como se esperaba, es decir, puede que hayan visualizado un solo pronúcleo, mas de dos pronúcleos (en casos de fiv) o ningún pronúcleo.
- DÍA 2: lo ideal en este momento es que el embrión cuente con 4 células.
- DÍA 3: una división perfecta seria que el embrión que teníamos con 4 células, cada una se duplicara, obteniendo 8 células.
- DÍA 4: es el día en el que el embrión nos da menos información. Es un momento clave en el desarrollo emrbionario ya que debe pasar de una conformación (en células) a otra algo mas compleja (mórula). Las células del embrión empiezan a “juntarse/fusionarse” dando un aspecto que nos aporta poca información a los embriólogos. Es el día que visualmente, peor se ve.
- DÍA 5: lo idea es que el embrión en este momento empiece a formar una cavidad para dar inicio a la formación del blastocisto. Podemos tener desde blastocistos tempranos hasta blastocistos expandidos (completamente formados). Este momento es uno de los mas indicados para realizar la transferencia embrionaria, ya que si el embrión ha llegado a la formación de blastocisto existe altas probabilidades de implantación.
- DÍA 6: El embrión debe ser un blastocito completamente formado o blastocisto en “hatching” esto quiere decir que la zona pelúcida se habrá agujeredado y comenzará a salir el interior del embrión para posteriormente implantar en el endometrio materno. El día 6 es el máximo que podemos tener en cultivo los embriones en los laboratorios de reproducción asistida. Los embriones que lleguen a día 6 en estadio de blastocisto y con buena calidad deben ser transferidos o vitrificados.
¿Qué significa que un embrión sea de grado A, B o C?
La sociedad española de fertilidad (SEF) y la asociación para el estudio de la Biología de la reproducción (ASEBIR) son dos grupos de interés que intentan unificar los criterios de clasificación de los embriones con el objetivo de que los biólogos de toda España valoren de forma uniforme a los embriones. Esto quiere decir que propone una clasificación basada en el número de células, número de fragmentos (restos de células), presencia de vacuolas, simetría y tamaño de las células, etc. En definitiva, atendiendo a una serie de características hacemos distinción entre 4 tipos de embriones:
- GRADO A: embrión que posee un numero de células acorde al día de desarrollo embrionario en el que se encuentra. No posee fragmentación, o es inferior al 11%
- GRADO B: tiene alguna célula mas o menos de lo que se supone normal y puede presentar algunos fragmentos (11-25%)
- GRADO C: Presenta del 26 al 35% de fragmentación y pueden aparecer otros orgánulos como vacuolas.
- GRADO D: Embrión muy fragmentado, donde en ocasiones puede confundirse las células con los fragmentos.
Esta clasificación, junto con el numero de células que tenga el embrión en cada día de desarrollo, nos puede dar un pronóstico de la tasa de éxito si lo transferimos al útero.
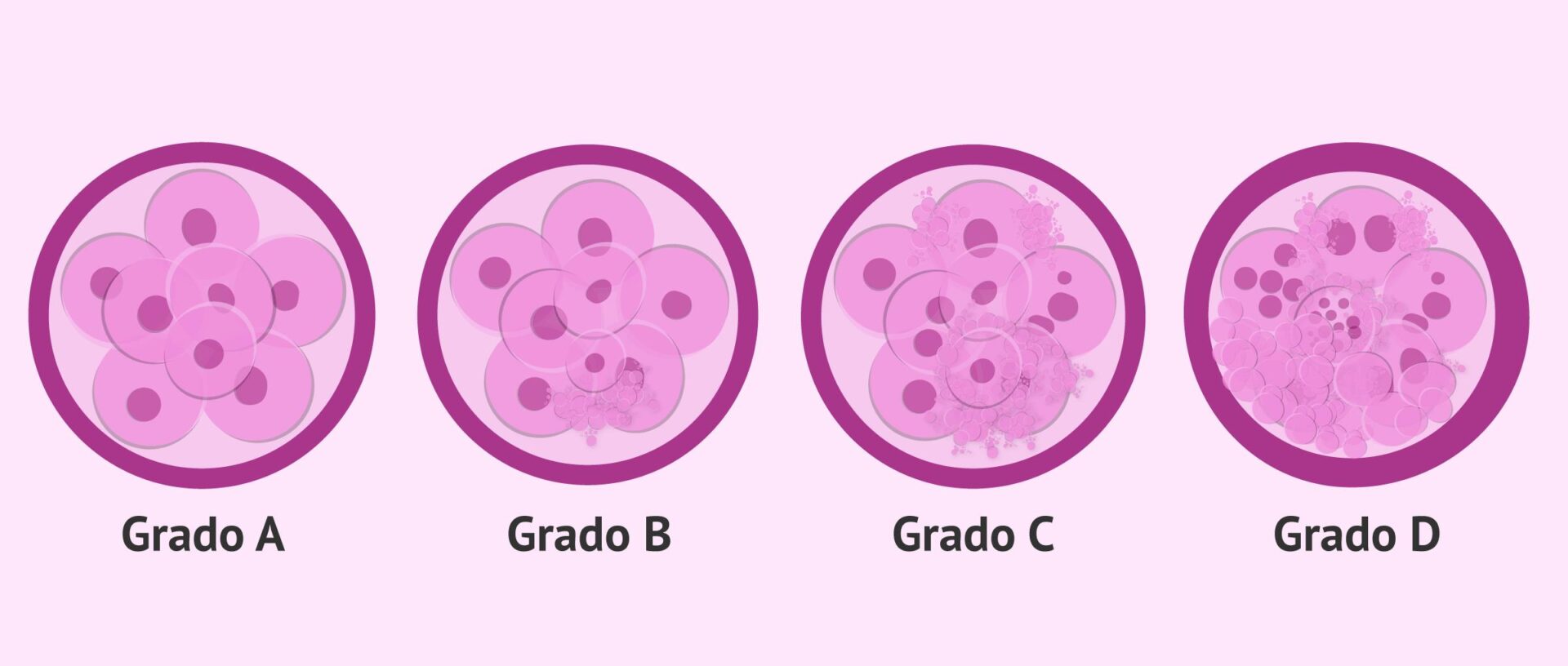
¿Un embrión de calidad C puede implantar? ¿Y de calidad A?
Si, puede implantar. La letra C se la otorgamos debido al ritmo de desarrollo y el aspecto que tiene visualmente. Tiene poder de implantación, pero tendrá un porcentaje algo menor que los embriones de calidad A o B.
¿Cuál es el mejor día para hacer la transferencia?
Para los embriólogos, decimos que el mejor día para realizar la transferencia embrionaria es el día 5. Esto es debido a que, como hemos tenido el embrión en cultivo durante 5 días en el laboratorio, hemos podido estudiar con detenimiento como ha sido su desarrollo, su velocidad de división, aspecto de las células, forma de la zona pelúcida o membrana.
Además, el paso de día 3 a día 4 es crucial para los embriones. Es el momento en el que los embriones empiezan a funcionar como una unidad y ponen en marcha una serie de mecanismos únicos de cada embrión. Aquí, desgraciadamente, se detienen muchos embriones porque no sigue en marcha las divisiones celulares. Es por eso que si transferimos un embrión en día 3 y no ocurre la implantación nunca sabremos si era porque el embrión se ha detenido o por otro factor.
En definitiva, en día 5 tenemos mas datos acerca del embrión que en día 3.
¿Qué es mejor transferir 1 embrión o 2?
Esta decisión en ocasiones es exclusivamente medica y en otras muy personal. Va a depender de las circunstancias y de la historia clínica de cada paciente. Es obvio que transfiriendo 2 embriones aumentamos la probabilidad de implantación, pero también aumentamos los riesgos de sufrir un embarazo múltiple. Esto, depende en que circunstancias es desaconsejable.
Dadas las tecnologías de hoy en día en los laboratorios de reproducción y las excelentes condiciones del cultivo embrionario en los incubadores, si transferimos un único embrión es porque pensamos que tiene potencial de implantación.
¿El embryoscope es imprescindible para mi tratamiento?
No, no es imprescindible. El Embryoscope es un incubador que proporciona miles de imágenes que una vez unidas se crea un video en el que el embriólogo puede ir visionando la división del embrión. Es una herramienta muy útil que nos ayuda a seleccionar el embrión con mayor calidad o potencial de implantación, pero no es imprescindible.
¿El desarrollo de los embriones es igual en FIV que en ICSI?
Si, la diferencia entre una técnica y otra es la manera en la que el espermatozoide ha fecundado al ovulo. En el FIV es de manera “natural” es decir, el óvulo se incuba con un número elevado de espermatozoides y aquel que consiga atravesar la membrana del ovulo será el que lo fecunde. Por tanto, aquí no hay selección del espermatozoide, sino que lo hace aquel más apto o que más conexión ovulo-espermatozoide ha tenido. Este es el método que tiene lugar de forma natural en las trompas de Falopio en el momento que una mujer ovula.
Sin embargo, en la ICSI es algo distinto. Es el embriólogo el que selecciona que espermatozoide entrará dentro del ovulo. Esta selección la hará teniendo en cuenta su movilidad y su morfología. Una vez seleccionado el más “apto” lo introduce en el ovulo con una fina pipeta de vidrio que atraviesa la membrana dejando al espermatozoide dentro del ovulo.
En los días posteriores el desarrollo debe ser el mismo independientemente de si es un embrión de FIV o de ICSI.
¿Por qué me tengo que hacer un ICSI y no un FIV?
Realizar una técnica u otra en principio es criterio del embriólogo ya que influirá en esta decisión la calidad de los gametos. Recomendamos FIV en pacientes jóvenes con un seminograma de buena calidad y sin patologías asociadas a los gametos.
Se deberá recurrir a la técnica de ICSI cuando contamos con un número de ovocitos escaso, el semen es de baja calidad o mala morfología, cuando después hay que realizar un Diagnóstico Genético Preimplantacional, o cuando hay antecedentes en ciclos previos de mala fecundación de los ovocitos.
¿Cómo se selecciona al donante de semen o donante de óvulos?
En los tratamientos en los que se precisa un donante de semen, una donante de óvulos o ambos gametos SIEMPRE se tiene en cuenta el fenotipo de la mujer que se somete al tratamiento y si tuviera pareja también el del varón. Es decir, se busca donantes que se asemejen en grupo étnico, color de piel, color de ojos, color y forma de pelo y en algunos casos se puede solicitar que sea del mismo grupo sanguíneo que la pareja o mujer que se somete al tratamiento.
DEPARTAMENTO DE BIOLOGÍA PHI FERTILITY
E. gonzálvez, embrióloga
Contacta con nuestra unidad de fertilidad.
Vithas Perpetuo Internacional. Plaza del Doctor Gómez Ulla 15, en Alicante.
Teléfono: 965230397 / +34 606437458
Email: info@phifertlity.com
Puedes seguir informado de nuestras publicaciones y noticias a través de nuestras redes sociales Facebook y Twitter.



